What are the principles of Good Digital Healthcare Design?
The broad role of digital healthcare design is progressing rapidly, driven by the need for digital and technological solutions to address the increasing challenges facing healthcare systems worldwide. Several barriers face digital healthcare solutions, such as compliance with healthcare regulations, clinical trials, and utilisation. On top of the factors affected by these barriers is the ability to innovate, which is the primary driver toward adopting digital healthcare solutions. In my previous article, What Are The Barriers to Medical Technology Innovation? I highlighted the barriers that face medical technology innovation. In her article for the HBR, Why Innovation in Health Care Is So Hard, Herzlinger shed light on the obstacles between healthcare and achieving innovation.
Unlike other industries, healthcare runs based on complex scientific and governmental regulations. While these regulations may vary in digital healthcare design solutions, they still present obstacles to expanding digital health applications. Given the nature of the industry, the last thing you need is to build a digital health solution that no one wants to use, which leads us to the digital health design and its importance as the user interface between the patient and the science (i.e. treatment, diagnosis and monitoring).
Digital Healthcare Design Principles
While there are general principles of good design, digital health design principles need to consider the nature of the targeted medical condition and adapt to the healthcare innovation pathway; below are the principles to consider during the design of digital health solutions.
Design with Patients: Find Their Real Needs
Focusing on the patient’s needs is one of the main pillars of innovation in the design thinking process (Design Thinking Guide: What, Why and How). However, the relationship between patients and the disease is unique and complex, such as in chronic diseases (i.e. chronic pain, hypertension, and diabetes). Designers and healthcare professionals should work together using qualitative and quantitative data to directly understand patients’ experience with the disease outside the clinic’s environment.
Digital healthcare design requires closing the gap between designers and patients by understanding the problem (Explore), identifying the solution (Develop), and checking The Double Diamond Design Thinking Process and How to Use it. This co-created design practice allows designers to understand patients’ nature through a field research practice. Healthcare providers need to appreciate this co-create nature of the process where different experts work together to close this gap through innovative digital health solutions that can be provided as a service to empower patients. Several tools and resources could be implemented to achieve this goal, such as:
- Draw it: The patient is asked to draw something related to the disease or the possible solution. This practice helps patients to express themselves and their personal experiences.
- Observation: This observation can be done by designers or by the patients (peer observation). In the peers’ observation, the patient observes other patients with the same condition (as participant or non-participant). As a result, the notes collected from the patient (observer) are influenced by the patient’s experience and accurately describe their practice.
- Card Sorting: This method allows the patient to describe their experience visually. For some patients, it can be challenging to describe their experience themselves. Therefore, other methods, such as card sorting, can be as effective. Check How to use the Card Sorting to Improve Service Design for more details about the tool and how it works.
- Think a Loud: This is a commonly used tool in user experience. In this tool, patients describe their experiences loudly. For example, they can describe the steps as they measure their blood sugar and describe their feelings as they move forward from one step to another.
- Storytelling: The storyboard is a flexible method as patients can use different tools to describe their health experience, such as using drawings, photos, or sampling to tell it in the form of a story.
Several tools can be used to involve patients in the design process. IDEO’s Design Kit (https://www.designkit.org/methods#filter) includes more tools that can be used in social research and innovation.
Video 1. How to use the Draw it tool in research (Source: IDEO page on Vimeo)
Adopt an Evidence-Based Design Process
The healthcare design regulations are complex and vary based on the medical intervention and the country. Generally, there should be an evidence-based mechanism to evaluate the efficacy of the digital health intervention. Accordingly, the design process should involve a similar mechanism to ensure that the product meets governmental requirements.
The principle of evidence-based design is not a common practice in the design industry. Usually, it is adopted in architecture and building healthcare facilities to ensure that the medical requirements key performance indicators (KPI) are considered and measured during the design process. The evidence-based process presents a link between science and design to ensure both sides acknowledge the outcome.
The evidence-based process varies in the type of the final product design and its impact on patient lives. For example, medical technologies used in surgical theatres have higher restrictions than the regulations used in public spaces. However, the efficacy evidence varies in its level of rigorousness. In her article, Weighing the Evidence, Jaynelle Stichler presented a hierarchy of evidence-based based on its strengths. This scale provides an opportunity for health technology companies to adopt their product to an accepted scientific evidence level. Stichler’s evidence level (Figure 1) is arranged into six levels, where level one is the highest credible and six is the lowest credible evidence.
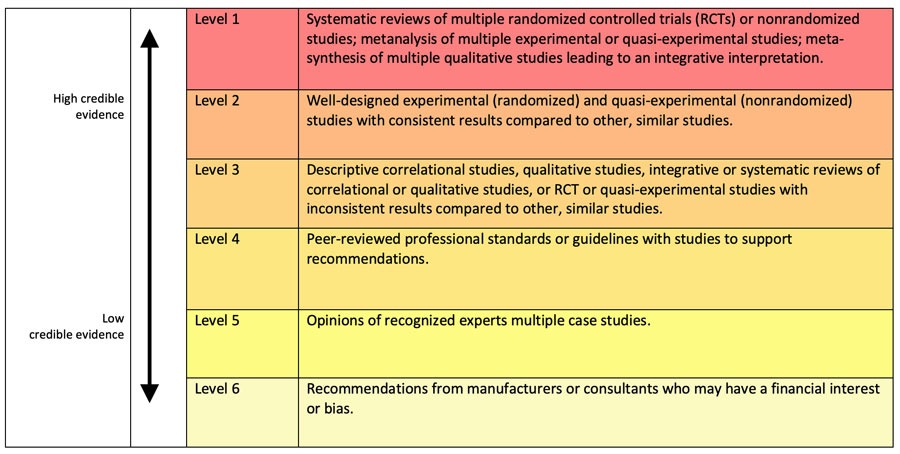
Adopting the above levels in testing and evaluating the health design allows companies to present credible evidence on the level of product credibility and how this may suit the target usage of the product or service.
Clinician-Patient Concordance Relationship
Healthcare systems like the NHS deeply acknowledge the confidentiality of information, even from patients themselves. This one-way relationship has several effects on patients, such as the lack of interest in adhering to the digital health solution. Another impact is the feeling of disconnection from the system that is supposed to support patients. This relationship is based on how the healthcare system works as a scientific, evidence-based industry. Patients are receptors of the treatment rather than a partner in a healthcare experience. The approach has several psychological and physical issues, as highlighted earlier.
Concordance is based on shifting from a one-way relationship to a two-way relationship between the clinician and patient. In this relationship, patients take part in the medical intervention plan and partly or fully administrate the treatment themselves (i.e., insulin pumps). Digital health enables this opportunity, such as health and virtual appointment apps. Allowing patients to view their health records and data helps them view their progress (exercise and weight loss mobile apps).
Consider Patient Adherence
Focusing on the patient’s needs alone is not enough. While user needs are one of three pillars of human-centred design, this factor alone is not enough in health technology, especially for chronic diseases and self-administered treatments. In these conditions, the magnitude of the time dimension is another challenge to build a user-centric solution. The focus on patient needs is no longer enough. The extent of adherence to the treatment duration, regardless of its length, is considered in the design process.
A clear awareness of the factors influencing patient usage and adherence to the intervention effectively addresses the factors driving patients to adhere to the medical treatment. Although different theories provide a detailed discussion of the different adherence factors and their applications, there is no systematic and practical method to help designers consider the appropriate adherence factors.
Video 2. The Adherence Canvas applies Evidence-Based Design principle (Level 5)
As part of my research at the School of Design, Northumbria University, I developed an Adherence Canvas tool (Video 2). The simple one-page canvas helps companies understand, consider, and measure the adherence factors while designing the health technology intervention. The canvas is free and can be downloaded from the Adherence Canvas website.
Design with the Context of Use in Mind
The term “context of use” is commonly used in user experience design to reflect the holistic experience that needs to be considered while designing digital health solutions. The context of use refers to the environment where the application is used. For example, designing applications displayed in public places (i.e. ATMs) is different from personal mobile applications as it needs to consider a higher level of security considerations and a more comprehensive accessibility range for users with disabilities.
In healthcare, the context of use takes an even more in-depth approach, putting into mind patients’ ability to use the intervention, the place where the application is used, and the surrounding environment. This consideration of the context of use cannot be achieved without contextual inquiry, in which the UX researchers investigate the environment that will surround patients when using the digital health solution. This field research can use various methods such as interviews, focus groups, observation, card sorting, shadowing and think-aloud.
Conclusion
There is a significant need for good digital health design in the healthcare industry, which faces stressful challenges. If appropriately applied, digital health design can address many of these challenges effectively. However, this goal cannot be achieved without appreciating the nature of the healthcare sector. As a scientific-driven sector, the digital health design should adopt the evidence-based design to indicate the credibility level of the digital health solution.
In addition to the adoption of evidence-based design, the focus of the patients should not only focus on their needs but also build a free information concordance communication between clinicians and patients. The third aspect considers the magnitude of patient adherence and its impact on patient adherence, especially for chronic and self-administered diseases. Extending patients themselves to consider the surrounding environment is another aspect of a reliable digital health solution. Qualitative contextual inquiry research should support this extension to the context of use.
Overall, a good digital health solution should consider integrating with the current evidence-based science and extending patient’s needs to consider communication and adherence needs.
Bibliography
Stichler, J. F. (2010). Weighing the Evidence. HERD: Health Environments Research & Design Journal, 3(4), 3–7.
Rodriguez, M. M., Casper, G., & Brennan, P. F. (2007). Patient-centred design: the potential of user-centred design in personal health records. Journal of AHIMA, 78(4), 44-46.
Vipond, D. (2018). Design principles for health and care. Access from: https://digital.nhs.uk/blog/transformation-blog/2018/design-principles-for-health-and-care. [Accessed on: April 2021]
Cama, R. (2009). Evidence-Based Healthcare Design. John Wiley & Sons.
Lorusso, L., Lee, J. H., & Worden, E. A. (2021). Design Thinking for Healthcare: Transliterating the Creative Problem-Solving Method Into Architectural Practice. HERD: Health Environments Research & Design Journal, 14(2), 16-29.
Healthcare design is an interdisciplinary practice where design is used to innovate in the healthcare systems, including service design. It uses design principles to solve healthcare challenges and provides innovative products and services.
1- Design with Patients: Find Their Real Needs
2- Adopt an Evidence-Based Design Process
3- Clinician-Patient Concordance Relationship
4- Consider Patient Adherence
5- Design with the Context of Use in Mind






